Know Your Density—
the life you save may be your own
Written by Ben Merrill Photos by Katherine Ives Photography
ARCHIVES
On July 14, 2020, Liane Willard was diagnosed with breast cancer.
“Seriously?” she asked her doctor. Ironically, her 3D mammogram report read,
“No Mammographic evidence of malignancy.” The result: normal. Clear without concern.
Recommendation—one year follow-up. “Seriously?” she asked her doctor again.
“There is something very wrong,” Liane explains, “when your 3D mammogram report tells you that everything is normal but a same-day ultrasound result reveals a suspicious mass. How is that possible? And how many other women have received the ‘good news’ from their mammogram report and gone about their lives as if everything is ‘normal’, when just below the surface—literally—the news isn’t good at all.”
Liane knows something about breast cancer. Her friend and fellow cancer survivor, Margie Singleton, had practically the same conversation with her doctor back in 2017. [Margie’s story was featured in our December 2020 issue of Reflections.] Just like Liane, Margie’s mammogram came back “normal.” And just like Liane’s, it was anything but normal.
When Liane scheduled her 3D mammogram in the summer of 2020, she made it clear to her OB/GYN that she also wanted an ultrasound—just to make sure. The OB/GYN (who also happens to be a friend) agreed to order an ultrasound because Liane’s breast density is a “D”.
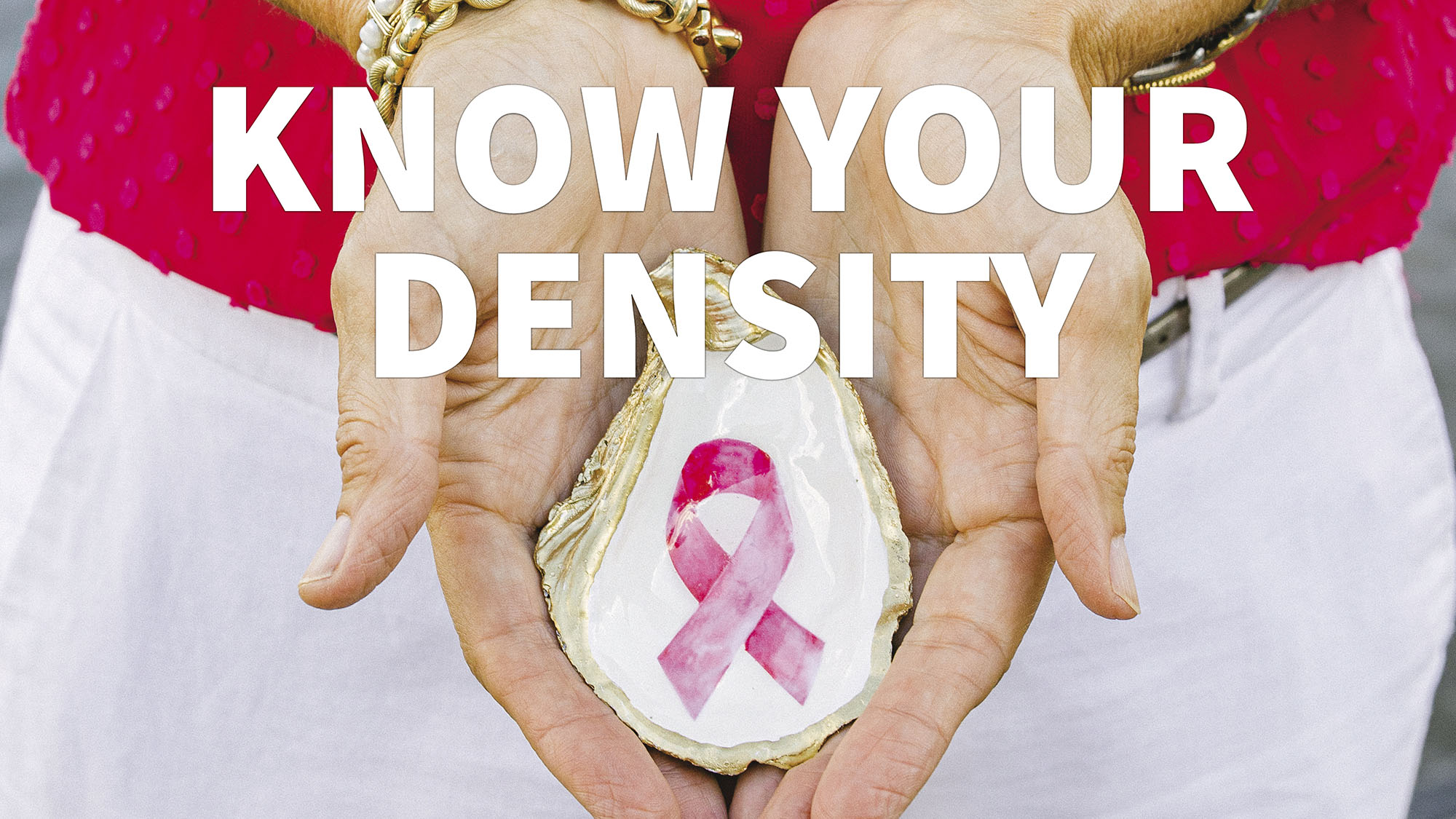
“Through my work with Margie,” Liane says, “I came to understand the seriousness of breast density. There are four levels —A, B, C, and D—and for women who fall in the C or D category, it is not only possible, but very likely that a mammogram may not pick up a small tumor lying deep within their breast tissue. Women with C or D breast density should not only be able to get further testing in conjunction with their mammograms, but it should be both encouraged and covered by insurance. Unfortunately, it is neither encouraged nor covered.”

Liane sits quietly on her back porch in the evening and watches as the moon comes up over the marsh. The rippling tides, gentle breezes, and rustling marsh grass remind her how fortunate she is not only to be alive, but also to be alive in such a beautiful, supportive, and caring community.
“I call it backyard therapy,” she says, “because sitting out here not only gives me perspective and a deep sense of gratitude, but also the quiet space I need to compose my thoughts, count my blessings, and [she takes a long pause here] plan my next steps.” Steps that include getting the message out in any way she can that it is time not only for women to take more control over their personal health needs, but also time for the medical community to step up and recognize that this is a very real problem.
“We aren’t talking about a random cases,” she says. “What we’re talking about is the simple fact that one in eight women will be diagnosed with breast cancer, and the majority of those women will have dense breast tissue. Knowing your breast density is as important as knowing your blood pressure and cholesterol levels. Heart disease is still the number one cause of death in Americans with cancer coming in second place. Failing to receive additional testing when you have dense breast tissue is a problem that the medical community—and the insurance industry—need to address.”
According to the Center for Disease Control (CDC), about half of women who are 40 years old or older have dense breast tissue that puts them at a higher risk of developing breast cancer. What’s more, dense breast tissue, which looks milky-white on a mammogram, can easily hide a tumor, especially if the tumor is small and just beginning to grow. For that reason, the CDC encourages women with breast density in the C or D range to request either an ultrasound or MRI to ensure their breasts are normal. Unfortunately, those requests are likely to be turned down by the medical community and almost certain to be turned down by the insurance companies.
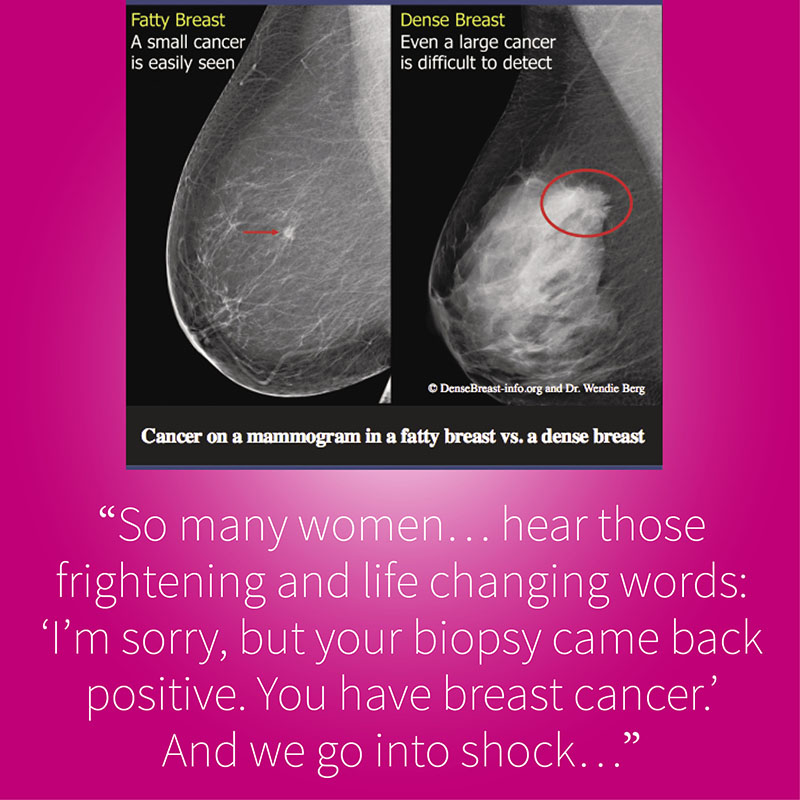
“So many women,” Liane says, “me included, hear those frightening and life changing words: ‘I’m sorry, but your biopsy came back positive. You have breast cancer.’ And we go into shock. We cry. We think about our families and our kids. We look in the mirror and ask ‘Why me?.’ Breast cancer is a life changing diagnosis. My life has forever changed and once I pushed past the shock and tears, I started looking in the mirror and asking, ‘Why NOT me?’ Because I realized—especially after working with Margie—that my cancer could be a catalyst for change. I could use my story to help others.”
“If I hadn’t had a personal friendship with my OB/GYN, the ultrasound would most likely have been denied, I would have simply received my ‘normal’ mammogram results and gone about my happy way. It might have taken two or more years for my tumor to grow to the point where it would be detected during a mammogram, and by that time, the cancer might have spread to who knows where. When my breast surgeon asked who ordered the ultrasound and I told him ‘Well, technically, I did,’ he responded, ‘Liane, you may have just saved your own life.’”
So what is the first step for any woman who learns she has dense breast tissue?
“Step one,” Liane says, “is to get your yearly 3D mammogram and do your monthly self breast exams. Step two is to ask what your breast density level is, and if you are a C or D density, ask your PCP or OB/GYN for further testing. Women who have a lower BMI are more likely than others to have dense breasts. If you get push back from your doctor, please advocate for yourself and insist on further testing—even when he or she tells you that your insurance company is most likely going to deny coverage.”
It’s been just over a year now since Liane learned she had breast cancer. Since her diagnosis, she’s received 18 Herceptin (antibody) treatments, chemotherapy, a lumpectomy, and 35 (7 weeks) proton radiation treatments. Proton radiation, something no one even told her about here in Savannah, has shown promise in treating several kinds of cancer, and according to the Mayo Clinic, studies have suggested that proton therapy may cause fewer side effects than traditional radiation since doctors can better control where the proton beams deposit their energy.
“But,” she says, “I wouldn’t have even known about proton therapy had I not received a second opinion at the Mayo Clinic in Jacksonville. If I’ve learned one thing on this journey over the past year, it’s that you have to ask questions. Are there other options? Are there other procedures? My message to any woman who is diagnosed with breast cancer is: ask questions, do your homework, and don’t take ‘no’ for an answer. In the meantime, I’m going to focus my energy on encouraging every woman I meet—and hopefully thousands of women I’ll never meet—to start demanding appropriate diagnostic procedures.”
It’s the end of another busy day and Liane is once again sitting on her back porch. The breeze off of the river is cooling, and the marsh grass almost shimmers in the setting sun. A great blue heron glides quietly overhead looking for its evening meal.
“I am thankful and humbled every day that I can sit here and enjoy this,” Liane says. “And insisting on that one little ultrasound could very well mean I’ll be sitting on this porch for years to come. That’s what I want. And that’s what I want for every woman. And with women advocating for themselves and asking for further testing, I know it can happen.”