The Other Side of Covid
One Family’s Story of a Miracle
WORDS BY BEN MERRILL PHOTOS BY THREE LINES CREATIVE

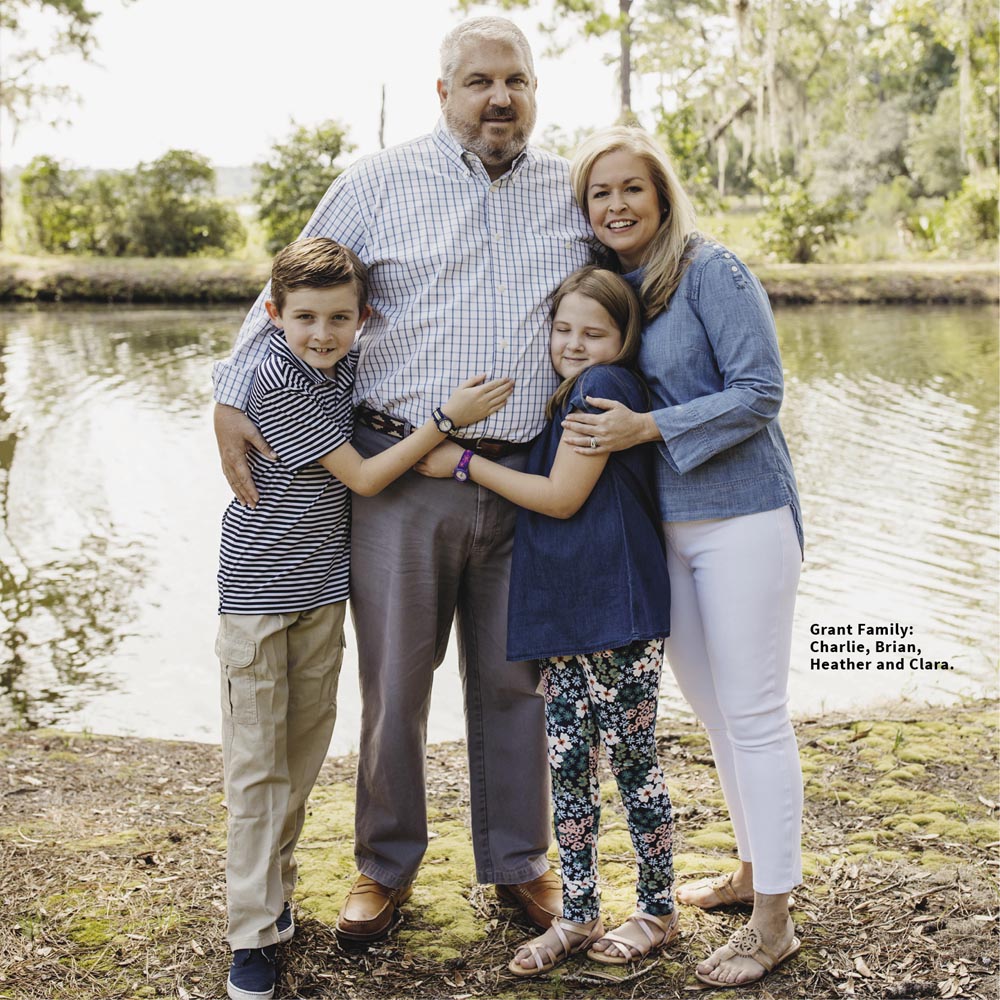
By February of 2021—a year into the Covid-19 pandemic—Brian and Heather Grant were feeling cautiously optimistic. Like millions of other Americans, they had taken every possible step to keep themselves and their children safe from harm. They wore masks in public places, they had their groceries delivered, they sanitized commonly used surfaces, and they socialized only within their pod. The vaccine wasn’t yet available for their age group but they closely monitored developments to know when they could receive it—just another step closer to normalcy. But then the unthinkable happened.
Brian Grant is tall and stocky. He and his brother, Scott, build solid houses designed to stand the test of both time and the elements. When you look at him, there’s no question in your mind that it would take a lot to bring him down. So when he got the chills, a headache, and some mild flu-like symptoms one day in early February, he wrote them off as a minor set back—an irritation. He had, after all, been working pretty hard lately. But he would soon find out this wasn’t just work fatigue—it was Covid-19.
Covid ultimately made its way through their family of four. Both children rebounded within a day or two, while Heather and Brian suffered severe flu-like symptoms, followed by several days of fatigue.
“I was really kind of shocked we all got it,” says Brian, “We couldn’t have taken any more precautions. But I’d also known others who’d gotten Covid and—not to downplay it—I figured I might be out for a couple of days. I wasn’t worried.”
“Brian’s barely been sick a day in his life,” says his wife Heather, sitting in the home they’ve shared for the past 13 years. “So it didn’t surprise me that a few days after initial symptoms set in he was back outside blowing the driveway and puttering around the yard. That’s Brian. But later that afternoon he started to look really tired. By the next day, he kept saying he couldn’t quite catch his breath. That was on a Thursday. By Sunday he was repeatedly saying he wished he had some oxygen.”
On Monday, Heather decided to take Brian to a doctor who put him on heavy steroids and breathing treatments to open up his air passages. But that didn’t work. On Tuesday, his breathing got so labored that she took him to the Emergency Room where he barely met the criteria, but nevertheless received a monoclonal antibody infusion. But that didn’t work either. On Wednesday, she took him back to the ER where they did a CT scan of his lungs. Based on what they saw—which was mostly positive—they sent him home again, this time with an oxygen machine.
“I cranked that machine to the max,” Brian says, “but it didn’t help. I’m not a guy who goes to the hospital. So for me, a trip to the ER is not good. Two trips to the ER is…well, this is a family magazine, so use your imagination. The thought of making a third trip to the ER—now I was beginning to get a little scared.”
“This so was unlike Brian,” Heather says. The next morning, he woke up completely drenched. But his temperature was only 96. That’s when it really dawned on me that something was very, very wrong. I watched his oxygen saturation decline by the hour. I didn’t know how to tell him that we had to go back—for a third time—to the hospital.”
“I remember it was Thursday evening,” she says, “and my options were rapidly dwindling. I finally told Brian we had to get help, to which he replied, ‘I can’t make it to the hospital without oxygen, call an ambulance.’ It was the most terrifying thing I’d ever heard. And just like that, he was gone.”
As Heather sat in an almost stunned silence that night, memories of their first blind date, the birth of their two children, family vacations, and the life they’d built together just washed over her. “It was the most frightening night of my life,” she says, her voice faltering. “All I kept thinking was, ‘I need him home.’”
At this point in our interview, Brian stops contributing. “I remember the ambulance ride,” he says, “and I remember hearing someone say ‘St. Joseph’s isn’t taking Covid patients’ but I don’t remember much else. We did, in fact, go to St. Joseph’s but then my lights just went out. I don’t have a single memory of anything that happened after that. Or for that matter, for the next six weeks.”
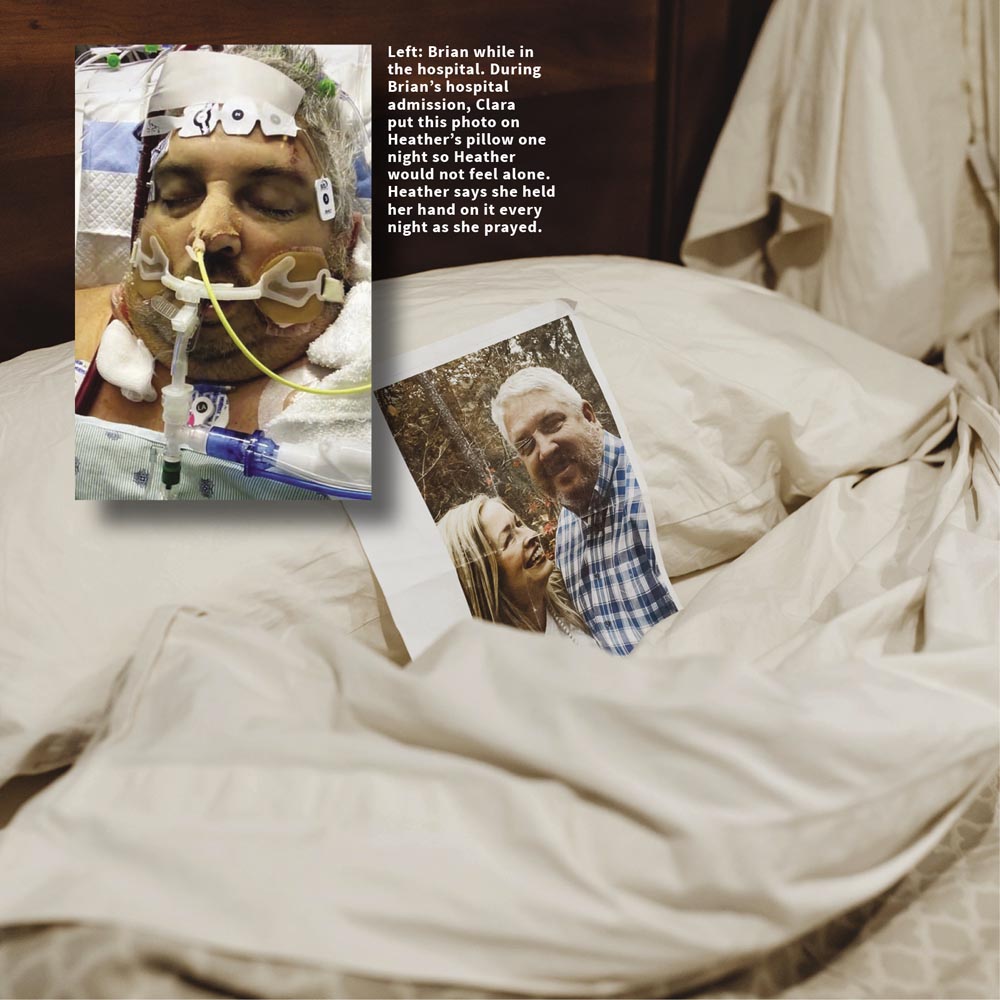
Heather, meanwhile, had two kids to comfort and a house to maintain. “They wouldn’t let me in to see him,” she says, “and that was really the hardest thing. The kids and I would form a prayer circle at night, and we’d pray for daddy’s quick return home. But there was schoolwork to do and other obligations that had to be met, and the days just inched along. I expected the phone to ring at any moment, but I didn’t allow myself to imagine what the news would be, good or bad. It was just the most stressful time of my life. Fortunately, we were blessed to have Brian’s parents, my parents, friends and family nearby who stepped in to keep things running, which allowed me to focus on Brian’s treatment and care.”
“Since I couldn’t be there in person,” Heather says, “I sent pictures of our family for the nurses to hang on his walls. I wanted them to see him not as another sick patient, but as a healthy 47-year old with a wife and two amazing kids that he needed to get home to. And God love them, with all of the demands they face, they hung the pictures. They were absolutely amazing, and it honestly gave me a glimmer of hope that we’d get through this.”
Two days later—it was a Sunday morning—Heather received a heart-stopping call.
“At this point,” Heather says, “they’d tried everything, but he just wasn’t responding. He had double pneumonia, Covid, and Acute Respiratory Distress Syndrome (ARDS), and it wasn’t looking promising. The nurse on the phone explained they were moving him from the seventh floor to ICU and intubating him to start him on a ventilator—he would no longer be breathing on his own. It was either intubate or sign a DNR (Do Not Resuscitate). I remember begging the nurses to do whatever they could, dropping the phone, sobbing and praying with my children, then reaching out to family in complete desperation and helplessness.”
“Before he had to be intubated,” she continued, her eyes tearing over (again), “he did call me a couple of times, though he has no memory of doing so. He was so exhausted that he would just fall asleep on the other end of the line. I would hold the phone and listen to him breathe—labored as it was—because it was the closest I could get to being by his side. I was still not allowed to visit him. I just sat there crying, praying, and listening, not knowing if I’d even have that privilege the next day.
Throughout the Covid-19 pandemic, most of us have heard stories about families having to watch from afar, as their loved ones are treated in the hospital, or worse, having to say goodbye forever to loved ones via apps like, FaceTime or Zoom. Some, like Heather, may have even endured similar circumstances. I took a moment to really think about how that would feel, being turned away at the Emergency Room by a security guard telling you you cannot go inside with your loved one, (your mom, dad, brother, sister, grandma or grandpa) at a time when you want and need to be there the most. A time when it may be your last chance to hold their hand, kiss their cheek or hug them to say goodbye. As the gravity of those thoughts settle, it feels like rocks in the pit of my stomach and the anxiety it invokes makes me quickly change my thoughts to something happy to rid myself of the inner discomfort associated with those feelings. I can only imagine the pain and fear these experiences truly cause, but just the feelings brought forth with imagining are enough to make me pray I never have to face a similar situation.
Five days after Brian was intubated—to no avail—doctors asked for Heather’s consent to put him on an extracorporeal membrane oxygenation (ECMO) machine, which pumps blood out of a person’s body, oxygenates it, and pumps it back in. Brian was only the second patient they’d done that to, and they made no secret about it that it was a last-ditch effort. The weeks that followed were a roller coaster ride. Brian would improve and then decline—sometimes by the day, sometimes by the hour.
“Then,” Heather says, “came the phone call I’d been dreading. It was 2:36am. It was the hospital and I feared the worst. As I sat there in the dark, the nurse explained that Brian’s vitals were falling and they needed my permission to scope his lungs. ‘Of course,’ I said. ‘Do whatever you can.’ Then I just sat there in my bed, praying, listening to praise music, and staring at the phone, waiting for an update. At 6am, they called to say that Brian had developed a massive nose bleed that had drained and nearly filled his lungs. He would undergo four scopes to remove clots that day—just one of the many ‘bumps’ on our journey. As we neared the end, his medical team was a mere day away from starting him on kidney dialysis. Despite being on both an ECMO machine and a ventilator, his body was struggling to combat all that was happening to it. I listened quietly as the doctor told me—as gently as he could—they were running out of options.”
And then the impossible happened.
“Against all odds,” Heather says, “Brian slowly began to turn the corner. I remember speaking with the wife of the only other patient who’d been on the ECMO machine, and she warned me that when he did wake up, it wasn’t going to be a Hallmark moment. It would be very gradual and it would take a lot of time. And she was right. Days went by where he’d be awake for a few moments before going right back to sleep. I just held his hand and waited. It would be a long wait.”
“It was probably towards the middle of April,” Brian says, rejoining the conversation, “nearly two months after they’d taken me away before I was really aware of what was going on around me. I couldn’t lift an arm or move a leg because my muscles had all atrophied, and I couldn’t speak because I was still on a ventilator with a tracheostomy. It would be another month before I’d be able to move enough to begin physical therapy. It took me two and a half months to learn how to walk again. But I was still here, and for that I was grateful.”
Brian finally made it home during the last week of May. It had been 94 days since that fateful ambulance ride, and he was still feeling incredibly weak. But it felt good to be home.
“Doctors are pragmatic people,” Brian says. “They know how the body works, and they know that despite their best efforts, it doesn’t always work out for the best. I was on two life support systems, and they were still losing me. They had tried everything in their toolkit, and nothing had worked. I have no doubt that making that phone call was as painful for them as it was for Heather. But God had other plans.”
“Every doctor, every nurse, has told us the same thing,” Heather says. “He’s not supposed to be here. They were referring to him as the ‘miracle guy’. And ‘miracle’ is not a word that doctors and nurses throw around lightly.”
Today, life at the Grant’s has mostly returned to normal. But it will never be the same. Brian is three months into what will likely be a yearlong recovery. Still, they have a new appreciation for each other, for their families, and for such a supportive community. The worst possible season of their lives has given them a new sense of God’s presence and power.
“You pray that your faith will never be tested,” Heather says, “but when it is, you come to understand just how precious life is, how grateful you are for the people He has put in your life, and the limitless power of God. The doctors, the nurses, our families, and the ‘village’ that sustained us, I have such a new appreciation for everyone and everything. I wake up every morning now and thank God for the beauty yet to come.”
You can follow Brian’s entire journey on Facebook via the group page “Bold Prayers for Brian.”